Abdominal Aneurysms (Descending)
Often called the “silent killer”, abdominal aortic aneurysms usually do not show any symptoms until rupture.
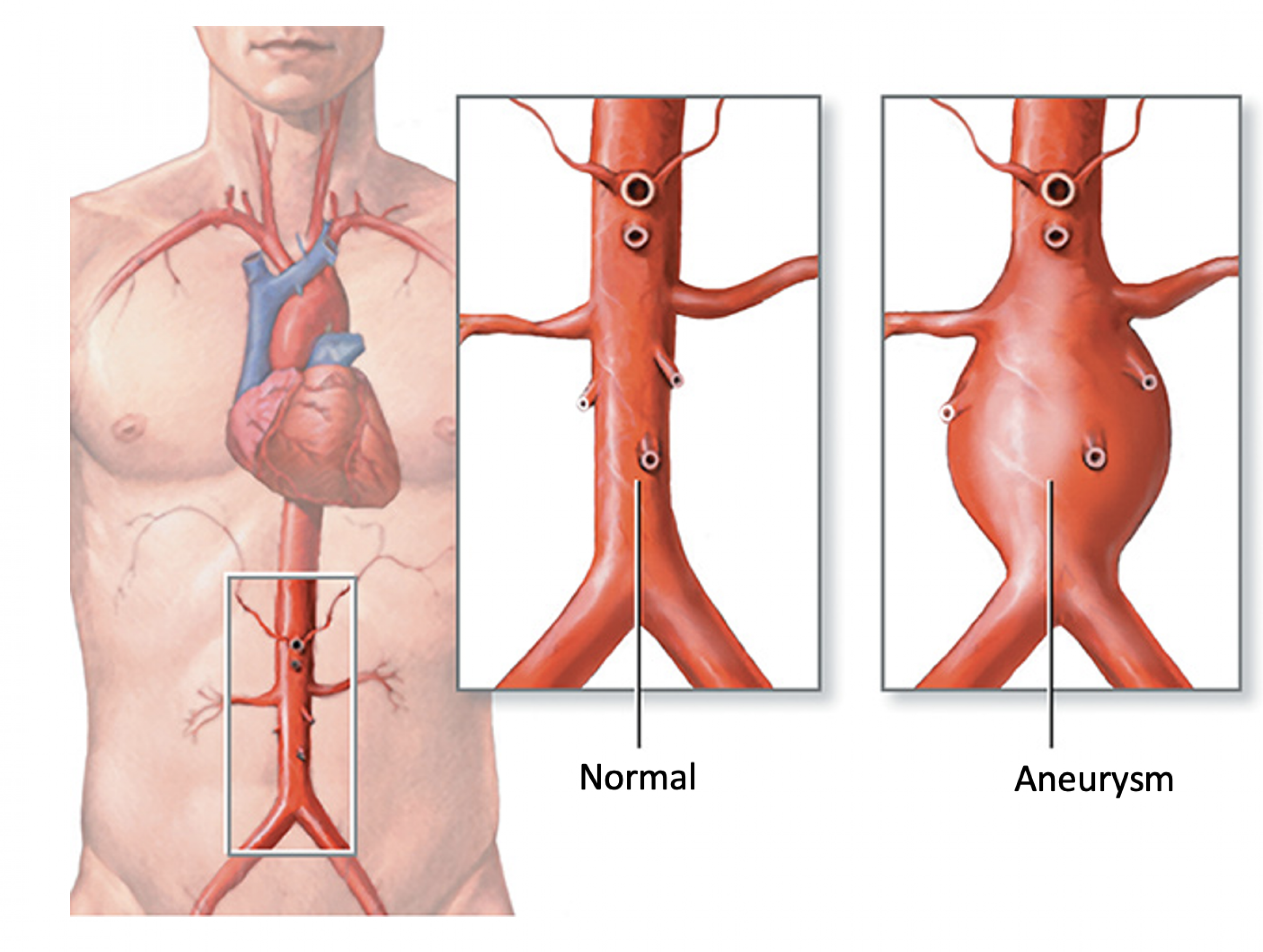 The aorta is the body's largest blood vessel and is responsible for carrying about 2000 gallons of blood from the heart to the rest of your body each day. The lower part of the aorta, in between the chest and the hips, is called the abdominal aorta. The abdominal aorta transports blood to the abdominal organs, pelvic organs, and your legs. Aging and certain risk factors make the abdominal aorta a common spot for aneurysm development. An abdominal aortic aneurysm (AAA) is a bulging or ballooning of the blood vessel which occurs when blood pushes against a weakened or damaged artery wall. If left unmonitored and/or untreated, an AAA may grow large enough to rupture. An AAA rupture is a serious medical emergency causing significant internal bleeding and possibly death. AAA rupture is the 13th leading cause of death in the United States.
The aorta is the body's largest blood vessel and is responsible for carrying about 2000 gallons of blood from the heart to the rest of your body each day. The lower part of the aorta, in between the chest and the hips, is called the abdominal aorta. The abdominal aorta transports blood to the abdominal organs, pelvic organs, and your legs. Aging and certain risk factors make the abdominal aorta a common spot for aneurysm development. An abdominal aortic aneurysm (AAA) is a bulging or ballooning of the blood vessel which occurs when blood pushes against a weakened or damaged artery wall. If left unmonitored and/or untreated, an AAA may grow large enough to rupture. An AAA rupture is a serious medical emergency causing significant internal bleeding and possibly death. AAA rupture is the 13th leading cause of death in the United States.
Risk Factors
There are many uncontrollable and controllable factors that put a patient at risk for AAA growth. As we age, our blood vessels begin to weaken and bulge, potentially causing an aneurysm. This is why most AAA’s occur in patients over the age of 50 years old. In addition, a family history of aneurysms is a strong predictor of aneurysm presence. Up to 30% of patients with an AAA have a first or second degree relative with an aneurysm. Risk factors such as smoking and high blood pressure can speed up the artery weakening process and cause AAA’s. People who smoke are about 7 times more likely to develop an AAA than people who do not smoke. If you have one or more of these risk factors you may be eligible for a screening AAA study.
- Advanced Age
- Family History of Aneurysms
- Tobacco Use
- High Blood Pressure
- Peripheral Arterial Disease
Symptoms
Often called the “silent killer”, abdominal aneurysms usually do not show any symptoms until rupture. As a patient with an AAA, it is important to understand the signs and symptoms of aneurysm rupture and growth. If you experience any of these symptoms call 911 right away.
- Severe abdominal pain
- Severe back pain
- Severe flank pain
- Pulsating sensation over the stomach
Diagnosis
Because abdominal aortic aneurysm’s (AAA) usually do not have any symptoms until rupture, AAA’s are often found as an incidental finding as a patient is undergoing tests for another health condition. In addition, AAA’s are discovered during screening studies for patients with risk factors for aneurysm development.
Here at BEVSA, our doctors and vascular technicians specialize in performing and examining diagnostic tests to assess our patients' AAA’s. Our team at BEVSA has specific training and experience in the natural history, medical treatment, minimally invasive repair and traditional surgical repair options for patients with an AAA. BEVSA is an optimal partner to help patients get the most thorough diagnosis, management, and treatment of their AAA.
Diagnostic Tests for AAA include:
Abdominal Ultrasound: This is a noninvasive, imaging study performed at our office that uses sound waves to visualize the aneurysm and assess its location and size. This is the most common test performed by our staff for patients with AAA’s and takes about 15 minutes. This study allows our physicians to monitor your aneurysm growth over time and make treatment decisions if necessary.
CT scan: This is an imaging study that combines x-ray technology and contrast use. The dye is injected through a small IV line started in your arm and the test does not require any sedation. This test is usually performed for patients with large, growing aneurysms to determine if they are a candidate for surgery.
Treatment Options for Small Aneurysms
For small aneurysms, it is important that a patient follows up with routine appointments at BEVSA every 6-12 months. These appointments allow the surgeons at BEVSA to obtain ultrasound scans of the AAA and track its size, shape, and growth over time. Failure to continue routine appointments with a vascular surgeon puts a patient at risk of delayed aneurysm treatment and potential rupture. In addition, we work with our patients to ensure they are making the appropriate lifestyle and medication changes to control modifiable risk factors such as smoking and high blood pressure
Treatment Options for Large Aneurysms
Due to a large, rapidly growing, or irregularly shaped aneurysm, your surgeon may determine that repair is necessary to prevent aneurysm rupture. Our surgeons at BEVSA specialize, and are well experienced in traditional surgical and new, minimally invasive options for aneurysm repair. We will work with you and your healthcare team to determine which treatment option is the best fit depending on the location of the aneurysm and surgical risks.
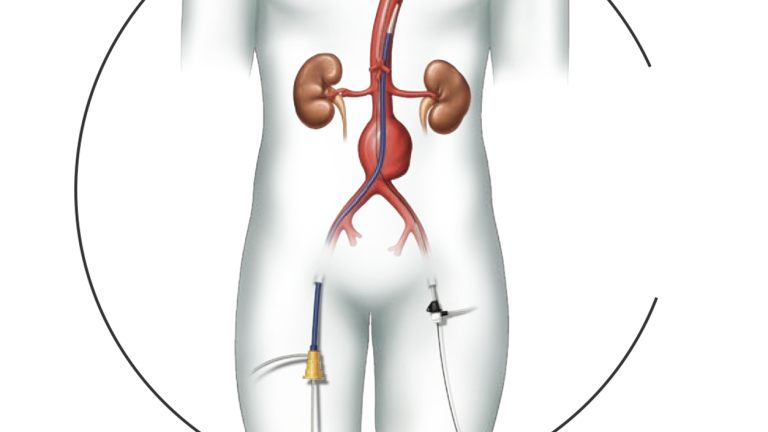
Endovascular Aneurysm Repair (EVAR): Until very recently, aneurysm repair was an extensive open surgery that required a large incision over the abdomen. However, EVAR is a new, minimally invasive option available to qualifying patients at BEVSA. The procedure involves two small incisions in the groin and delivery of an endograft to the aneurysm by a delivery catheter (long tube). Once the endograft is placed over the aneurysm, it directs blood flow through the graft to ensure your legs receive blood. The endograft also blocks off blood flow into the aneurysm sac. This prevents further weakening and growth of the aneurysm wall and decreases the risk of rupture. The procedure is usually 2-4 hours and most patients are put under general anesthesia and discharged from the hospital in 1-2 days. For more information about the patient EVAR experience at BEVSA, click on the aneurysm repair patient video below.
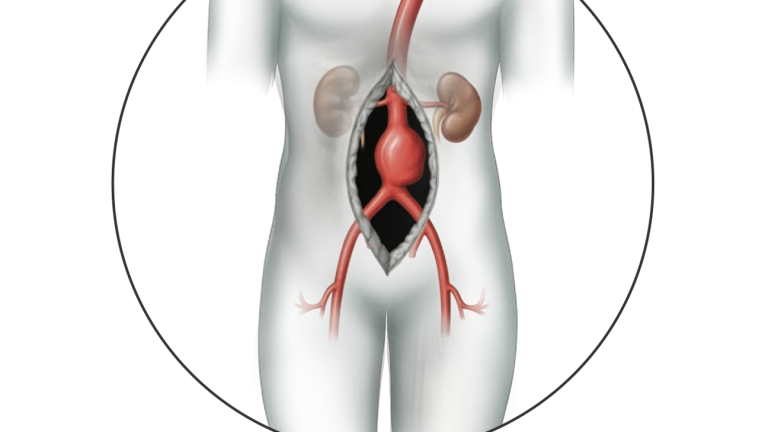
Open Abdominal Aneurysm Repair: Open aneurysm repair is a 3-4 hour procedure under general anesthesia that involves the surgeon making a cut across your abdomen. The aorta is exposed and the aneurysm is then manually removed from the blood vessel and replaced with a graft. The graft is sewn to the aorta and acts as a replacement vessel for blood to flow through as it travels down the aorta. Direct removal of the aneurysm from the aorta prevents rupture in the future. This is a more extensive procedure usually reserved for patients with complex aneurysms who do not qualify for a minimally invasive option and requires about a week in the hospital to recover.
Frequently Asked Questions
What are the potential benefits and risks associated with open aneurysm repair?
Open aneurysm repair is the traditional treatment option for aneurysms, and is a well proven surgical treatment with extensive amounts of data. Data shows that this procedure has very good long term outcomes and a decreased likelihood of patients needing a subsequent procedure after their initial surgery when compared to EVAR. Drawbacks of this procedure are an extended surgery length, higher surgical complication rate, and longer recovery than EVAR.
What are the potential benefits and risks associated with endovascular aneurysm repair (EVAR)?
EVAR is a new, minimally invasive treatment option that requires a smaller incision, shorter surgery duration, less risk of surgical complication, and shorter recovery time when compared to open repair. Drawbacks of this procedure are a higher rate of graft complications and possible additional minimally invasive graft repair surgeries when compared to open repair.
Do I need to follow up with my vascular surgeon after aneurysm surgery?
After your aneurysm repair, it is critical to follow up with your surgeon so they can examine your incision sites and check to ensure your graft is placed correctly and functioning well. After your first check-up appointment, your physician will likely want to see you every 6-12 months with CT scans or ultrasound studies to measure the size of your aneurysm and ensure it is not growing. Sometimes, if a leak is discovered in the graft, an additional procedure may be necessary to lessen the risk of aneurysm rupture. Patients who fail to follow up with routine appointments are at a heightened risk of aneurysm rupture since we cannot identify and treat any potential problems early on.
Treatment Options for Abdominal Aneurysms (Descending)
Descending Endovascular Aneurysm Repair (EVAR)
- Minimally Invasive
- Endograft Placement
- Aneurysm Rupture Prevention