Aortoiliac Occlusive Disease
Aortoiliac Occlusive Disease is a subtype of peripheral arterial disease describing a high degree of narrowing or blockage of the lower aorta and iliac arteries.
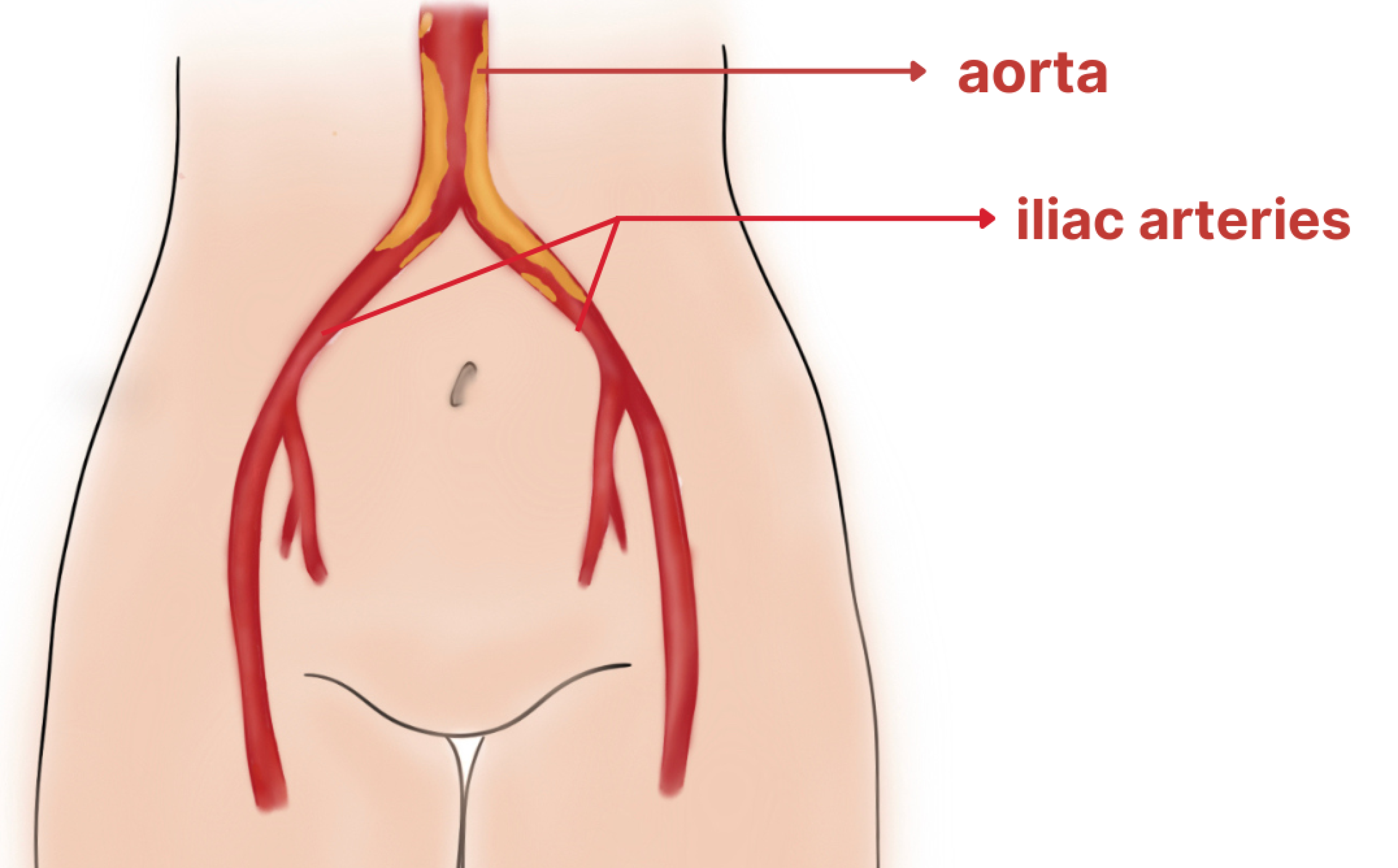
The aorta is a major artery that comes off the heart and travels down the abdomen and branches into the iliac arteries to supply the legs with blood. When plaque builds up in these arteries, it can reduce blood flow to other regions of the body, and result in leg pain and erectile dysfunction in men.
Risk Factors
Many controllable lifestyle choices and uncontrollable factors such as genetics and aging can put a patient at risk for aortoiliac occlusive disease.
- Advanced Age (over 50 years old)
- Family History of PAD, Stroke, Heart Disease
- Diabetes
- Smoking (Current smoking or history of smoking)
- High Cholesterol
- High Blood Pressure
- Coagulation disorders
- Obesity
- Personal History of Stroke, Heart Attack
Symptoms
Depending on the progression of your aortoiliac disease, symptoms can range from minor leg pain while walking to severe persistent pain and coolness in your legs and feet. The aorta and iliac arteries direct blood to the legs, and blockage in these regions can cause a range of symptoms in the abdomen, back, flank, and legs.
Early Symptoms:
One of the earliest signs of plaque buildup in the aorta and iliac arteries is claudication. Claudication is fatigue, pain, or cramping in the buttocks, thighs, or calves when walking while walking–on flat surfaces, up an incline, or when carrying heavy weights. Most commonly, people have a hard time grocery shopping or carrying groceries to the car.
This pain usually disappears when the patient rests for a short period of time. Claudication is the result of a supply and demand imbalance. While walking, your muscles require more blood and oxygen; however, plaque in the arteries blocks the amount of circulation to the muscle and results in muscle fatigue and cramping. Once you rest and stop walking, the demand is not as great, and symptoms are resolved.
The location of the cramping and pain usually depends on the location of the clogged artery. One of the most common types of claudication is hip and buttock cramping while walking. The severity of claudication depends on the severity of the blockages with some patients able to tolerate their pain and others not being able to walk at all. Regardless of the severity, claudication is an important sign of aortoiliac disease and should be monitored and possibly treated by a vascular surgeon.
In addition, blockages in the aorta and iliac arteries can cause leg wounds and impede healing. This is because there is an inadequate supply of blood and important healing factors to the wound. If you have a wound that has not healed for over a month, and one or more risk factors for aortoiliac disease, it is important that you are screened. In addition to claudication and non healing wounds, hair loss on the legs, slow growing toenails, and coolness in the legs and feet are indicators of possible aortoiliac disease.
Advanced Symptoms:
If early signs and symptoms of aortoiliac disease are ignored or left untreated, it may develop into critical limb ischemia. Critical limb ischemia is when there are severe, and usually multiple, blockages in the leg arteries which significantly reduce the amount of blood reaching the foot. This usually results in rest pain. In acute ischemia cases, some patients experience numbness, tingling, pain, and burning sensation of the feet at rest. This is because the patient is not receiving an adequate supply of blood to the foot which results in nerve damage. Rest pain often affects patients' ability to sleep. Patients often report alleviation of their symptoms when they hang their foot over the side of the bed to increase blood flow to the foot. Critical limb ischemia also can result in coolness of the feet, ulcer formation, gangrene (black skin) of the legs, feet, toes. If you are experiencing any of these symptoms it is very important that you meet with a vascular surgeon right away.
Diagnosis
Here at BEVSA, our doctors and vascular technicians specialize in performing and examining multiple diagnostic tests to assess our patients' circulation.
Ankle-Brachial Index Test (ABI): The ABI test is a quick screening tool performed by our technicians that compares the blood pressure of the arteries at your ankle to the blood pressure of the arteries in your arm. If the pressures are the same, the patient has an ankle:brachial ratio of 1 and has normal circulation. In patients with aortoiliac disease, the blood pressure at the ankle is less than the blood pressure in the arm due to blockages in these arteries. This gives an ankle:brachial ratio less than 1. The lower the ratio, the more arterial disease present. This is one of the most common PAD tests performed at our office and takes about 5 minutes.
Arterial Ultrasound: This is a noninvasive, imaging study performed at our office that uses sound waves to visualize blood flow in the aorta and iliac arteries for signs of narrowing. This is one of the most common PAD tests performed at our office and takes about 10 minutes.
CT Angiogram Scan: This is an imaging study that combines x-ray technology and contrast use. The dye is injected through a small IV line started in your arm and the test does not require any sedation. This test is usually performed for patients with high grade artery narrowing to determine if they are a candidate for surgery.
Aortogram: This is a minimally invasive procedure performed at our office in which a catheter tube is inserted through a small incision in the leg to inject contrast dye into the aorta, iliac, and leg arteries. This test is often performed for patients after their screening studies have shown evidence for aortoiliac disease. An angiogram allows our surgeons to obtain “real time” views of the blood vessels with x-ray imaging. The procedure involves local sedation and takes 1-2 hours.
Nonsurgical Treatment Options for Aortoiliac Disease
For patients with mild to moderate aortoiliac disease, our physicians and team at BEVSA work with you to develop a treatment plan to prevent the progression of your disease.
Risk Factor Modification: Smoking and diabetes are the two most critical, controllable risk factors that patients with aortoiliac disease need to control. Tobacco use damages the arterial walls which makes it easier for plaque to build up and cause complications such as leg pain, non healing wounds, and amputation. More than 80% of patients with aortoiliac disease are current or former smokers. If you need help quitting smoking, our physicians will help you obtain information on medication, nicotine replacement products, and programs to make it easier
In addition, diabetes raises blood sugar levels which can damage the vessel walls and cause plaque buildup. People with diabetes are also prone to developing foot ulcers and toe gangrene which may require vascular attention to help with healing. Our physicians will work with you to make sure your blood sugar levels are stable and diabetes is well controlled.
Diet: Two of the main ingredients in plaque are cholesterol and fat. Therefore, It is important to maintain a diet low in saturated fat, cholesterol, and sodium. Foods with these components can elevate cholesterol levels making it more likely for plaque to build up in the arteries and cause narrowing. Our physicians will work with you to develop a customized, feasible, heart healthy diet plan.
Medication Management: Risk factors include elevated cholesterol/fat levels and type 2 diabetes. Statins have been shown to manage cholesterol/fat levels, stabilize plaque, and reduce the risk of plaque buildup. In addition patients with type 2 diabetes should engage in good glycemic control and work with their physician to achieve low levels of A1C. Our physicians will work with you to ensure you are on the proper medication regimen to lessen your risk of aortoiliac disease.
Surgical Treatment Options for Aortoiliac Disease
For patients with severe aortoiliac disease, our physicians and team at BEVSA work with you to treat your condition.
Minimally Invasive Procedure: This is an aortogram procedure performed at our office that only involves a small incision in the leg. A catheter (long, flexible tube) is then inserted in the leg to inject contrast dye into the aorta, iliac arteries, and leg arteries. The dye and real time x-ray images are used to identify where blockages in the arteries are occurring. After a blockage is identified, the vascular surgeon may use angioplasty, stenting, and atherectomy to improve circulation. Angioplasty is when a small balloon is inflated inside of the vessel to widen it. A stent, which is a hollow, metal scaffold, is sometimes placed permanently inside the artery to hold it open. There are also drug eluting stents which release drugs that fight any further plaque buildup in the stent itself. Our BEVSA practice is one of the leaders in the region at safely and effectively performing these procedures outside of the hospital at our specialized outpatient procedure facility, Access Care Vascular. The procedure takes about 1-2 hours and only requires local sedation. Patients are discharged home the same day as the procedure.
Endarterectomy: This is an open surgical procedure performed at Buffalo General hospital for patients that usually have full blockages of their aorta or iliac arteries that cannot be treated with a minimally invasive procedure. The endarterectomy procedure involves making an incision in the lower abdomen or groin. The artery is then clamped shut to prevent any blood flow through the diseased area. The diseased portion of the artery is then manually opened and plaque is removed with specialized tools. Afterwards, the artery is sewn shut and the clamps are removed. Blood is then able to pass through the once blocked portion of the artery and circulation through the aorta and iliac arteries is improved. This procedure is 1-2 hours and is sometimes paired with an angioplasty and/or stenting procedure if there are additional blockages present at harder to reach locations.
Surgical Bypass: This is an open surgical procedure performed at Buffalo General Hospital for patients that have full blockages of their aorta or iliac arteries that cannot be treated, or have failed to be treated, with a minimally invasive or endarterectomy procedure. A bypass graft is sewn above and below the diseased portion of the artery. This re-routes the blood around the blocked portion of the artery and creates better circulation for the legs. The bypass graft is either an artificial tube or a vein taken from the patient's leg. This is an extensive, lengthy procedure that requires general anesthesia.
There are several types of surgical bypass that are done, depending on the location and extent of aortoiliac occlusion.
- Aortoiliac bypass
- Bi-iliac aortoiliac bypass
- Fem-fem bypass
- Axillofemoral bypass
- Axillobifemoral bypass