Thrombectomy and Venous Stenting
Minimally Invasive Treatment Options for Your Veins
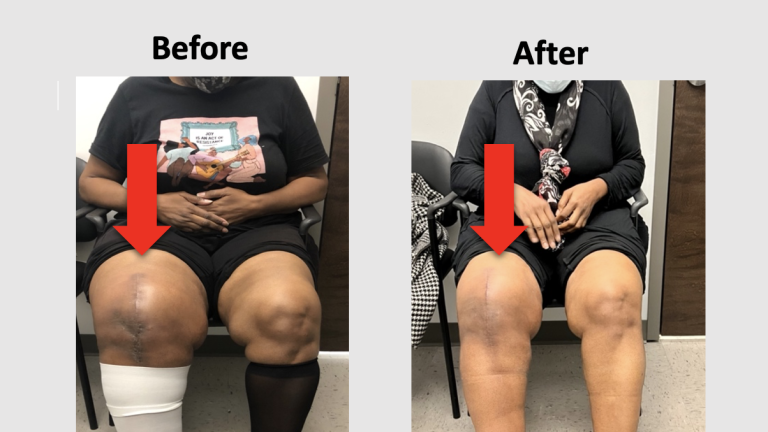
We are excited to offer you numerous, minimally invasive treatment options to alleviate swelling, tightness, heaviness, and discomfort in your legs due to venous disease. Our surgeons are always keeping up with the latest clot removal technology options, and we will listen to your story and analyze test results to assess which option works best for your needs. We perform select procedures safely and effectively at our outpatient procedure lab, AccessCare Vascular, as well as Buffalo General Hospital.
Who is Eligible for a Venous Procedure?
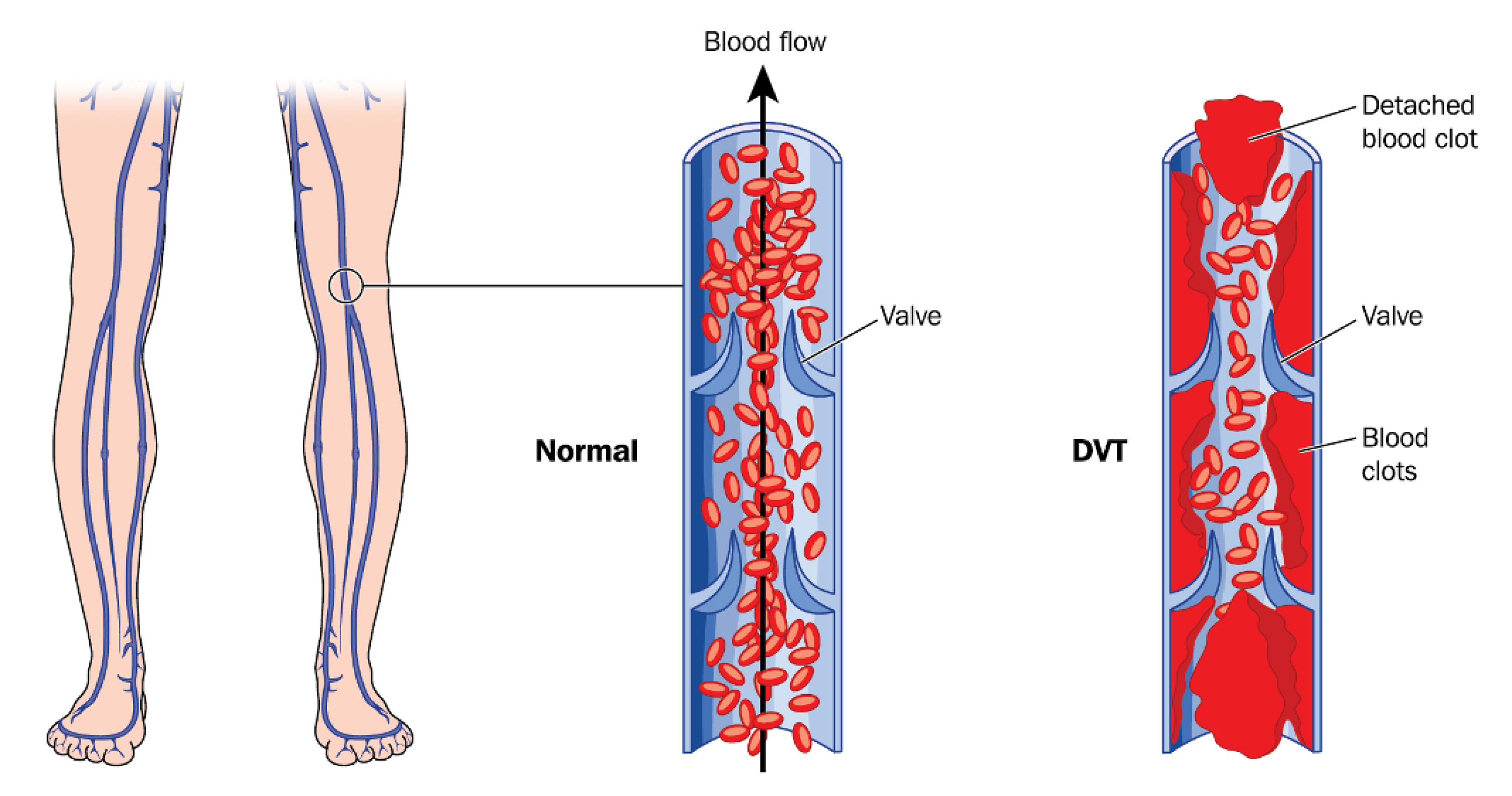
A deep vein thrombosis (DVT) is a blood clot that occurs in the veins. The clot can either partially or fully block the vein from being able to transport blood out of the legs. This causes symptoms in the legs such as swelling, skin tightness, and heaviness. A venous clot can also break off of the vein and travel to the lungs causing a life threatening condition called pulmonary embolism.
Patients with leg swelling and additional symptoms will first undergo a noninvasive imaging study, venous doppler, to assess the extent and location of the clot in their leg veins. Afterwards, your vascular surgeon will analyze the studies and listen to the severity of your symptoms to determine if you are eligible for a clot removal procedure.
Venous dopplers will help the surgeon assess if your DVT is above or below the knee. If your DVT is located below the knee, it is usually treated non surgically with blood thinners and leg elevation. This is because the risk of the clot breaking off and traveling to the lungs is low, and the the veins are usually too small to guide wires and clot busting devices through them. Above the knee DVT can be surgically treated because this condition poses an increased risk of significant swelling, pain, and pulmonary embolism. In addition, the veins above the knee are large enough for surgery.
Timing is also another crucial component to be eligible for a procedure. Usually, clot needs to be less than a couple of months old for a successful procedure. This is because the new clot is fresh and squishy and can be removed easily. If a clot is chronic, and has been in the vein for a long time, it becomes hardened and entrenched in the vein and cannot be removed.
Minimally Invasive Treatment Options
Diagnostic Venogram: A venogram is usually the first step of any venous procedure. This step is used to visualize the flow in the vein and the precise location of treatable blood clots. A small incision is usually made behind the knee to access the vein. A catheter (long, thin tube) is then guided through the puncture site. Next, contrast dye is injected in the vein and visualized using x-ray technology. In addition, a specialized catheter with an ultrasound device at the tip may be placed in the vein to visualize the inside of the vein and perform measurements. Combined, these imaging studies allow the surgeon to assess the location and extent of the venous clot and plan a treatment. The venogram is followed by a combination of thrombolysis, thrombectomy, and/or venous stenting.
Thrombolysis: Thrombolysis is a procedure in which a small puncture is made in the back of the knee to access the vein. A catheter (long, thin tube) is then guided through the puncture to the site of the clot. “Clot busting” medication is then delivered to the DVT in the vein to dissolve the blood clot and re-open the vein. Sometimes, a small device is inserted in the vein to mechanically break up the clot and/or a stent is placed in the vein to keep it open and prevent swelling. This procedure occurs at Buffalo General Hospital and usually requires a patient to stay overnight to allow the clot busting medication to fully dissolve the clot.
Thrombectomy: Thrombectomy is a procedure in which a small puncture is made in the back of the knee to access the vein. A catheter (long, thin tube) is then guided through the puncture to the site of the clot. A small device is then guided on the catheter to the site of the clot. The device is then controlled by the vascular surgeon to mechanically break up, collect, and remove the clot. This procedure can be performed on its own or after a thrombolysis in the hospital. In addition, thrombectomy can be performed safely and effectively at our outpatient facility, Access Care, with discharge home the same day.
Venous Stenting: In addition to a blood clot, sometimes patients with a DVT have an underlying compression of their vein. A compressed vein limits blood flow out of the leg, and can cause increased swelling even after the blood clot is removed. Therefore a stenting procedure is performed where a small puncture is made in the back of the knee to access the compressed vein. A catheter (long, thin tube) is then guided through the puncture to the narrowed vein. A stent is then guided along the catheter and placed inside the vein. The stent can help alleviate swelling and prevent blood from pooling in the veins and causing an additional DVT.
Angiojet Thrombectomy Procedure
This is an example of a minimally invasive treatment procedure for patients with DVT. The thrombectomy procedure uses a device that travels over the clot in the vein and aspirates, or sucks, clot out of the vein to open up the vein and reduce leg swelling.
Mechanical Thrombectomy
This is an example of a minimally invasive treatment procedure for patients with DVT. The mechanical thrombectomy procedure uses a device that breaks the clot and collects it in a wire structured bag to physically pull and remove the clot from the vein.
Procedure Details
For Hospital Procedures: Depending on the extent, location, and age of the clot, some patients are required to stay overnight at the hospital for a thrombolysis before the clot is removed. The thrombolysis procedure softens the clot, and the following day the clot can be removed by thrombectomy. Most of the procedures require the patient to lie flat on their stomach and the surgeon makes a small incision behind the knee to access the vein. A sedative is given to the patient which relaxes them and numbing medication is applied behind the knee to prevent any pain with the incision. After the clot is removed, sometimes a stent is placed in the vein to keep the vein open and improve flow. The procedure usually takes 1-2 hours. After the procedure, patients are transferred to a recovery floor where they are monitored anywhere from a couple of hours to an additional overnight stay. Patients are usually discharged on blood thinners to prevent any further DVT formation.
For AccessCare Procedures: Patients arrive the same day as their procedure, usually 1-2 hours before. They are taken to the recovery bay where their vitals are taken and the proper medication and fluids are administered. A sedative is given to the patient which relaxes them and numbing medication is applied behind the knee to prevent any pain with the incision. The patient is then transferred to the procedure room where the surgeon makes a small, minimally invasive incision behind the knee. The patient will need to lie flat on their stomach for the procedure which is usually 1-2 hours. Afterwards, the patient returns to the recovery area for 2-4 hours of monitoring by our nursing staff. Patients are then able to be discharged home the same day and will require someone to drive them home. Patients are usually discharged on blood thinners to prevent any further DVT formation.
Conditions Treatable with Thrombectomy and Venous Stenting
Deep Vein Thrombosis (DVT)
- Leg swelling
- Leg heaviness, discomfort
- Blood clots, pulmonary embolism
Learn More
May-Thurner Syndrome
- Iliac vein compression syndrome
- Venous insufficiency
- DVT
- Leg swelling